Provisions to MAPD Program Proposed Rule Impacting Star Ratings (CMS-4201-P)
This is an AArete Healthcare Payer insight
On December 14th, 2022, the Centers for Medicare & Medicaid Services (CMS) released a proposed rule that includes provisions to the Medicare Advantage (MAPD) Star Rating Program, and other provisions impacting MAPD beneficiaries. The proposal aims to improve timely access to care and behavioral health services, updates marketing guidelines, as well as measure additions, updates, and Star rating changes that impact health plan outcomes and revenues.
Select proposed rules are poised to shake up the industry Stars Performance in the following areas:
- Modifying the improvement measure Hold Harmless Policy to only 5-Star rated plans
- Reducing the weight of patient experience/complaints and access measures from 4 to 2
- Awarding Health Equity Index (HEI) rewards to incentivize plans to focus on Social Risk Factors (SRF)
- Removing recent cut point guardrails for non-CAHPS measures
Impact of the Improvement Measure Hold Harmless Provision:
-0.2 Star
Avg. Point Reduction
20%
4/4.5 Star Plans at QBP Risk
The initial Hold Harmless provision was introduced in 2018 and applied to 4.0 rated or higher plans. It registered the “better” number of the overall score, with 5 weighted improvement measures included and without. The new proposed rule removes the “better-of” language for 4.0 and 4.5 Star plans in order to continue to encourage improvements to a 5 Star plan.
This has the greatest impact to Quality Bonus Payments (QBP) and 4.0 and 4.5 rated plans. About 20% of 4.0 and 4.5 Star rated plans in 2023 would have been impacted and reduced to 3.5 or lower, removing their 5% QBP, estimated at $1.5 billion in reduced bonuses.
CMS estimates this to have $19 billion in 10-year savings.
Need a solution for your health plan? See what AArete can offer to address these challenges.
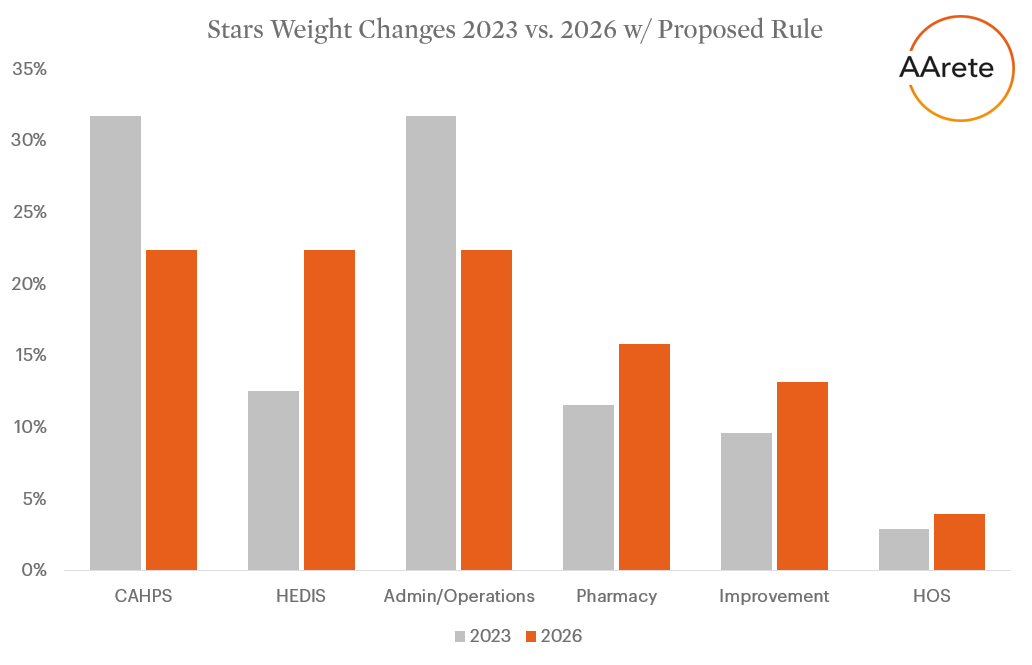
Reduced Measure Weights for Patient Experience/Complaints & Access
CMS previously increased select measure weights, from 2x to 4x, to improve member experience in Star Rating Year 2023. The proposal from December 14th, 2022 reverses that ruling and creates a more balanced program with process and outcomes measures. Plans should continue to focus on member needs and experience resulting in improved plan performance, provider experiences, and member healthcare outcomes.
New Weighting Criteria:
- 2x – Patient Experience/Complaints and Access Measures (CAHPS, Appeals, Complaints, Disenrollment, TTY), previously 4x
- 3x – Intermediate Outcome Measures (Pharmacy, HEDIS)
- 1x – Process Measures (HEDIS, HOS, Pharmacy)
- 5x – Part C and D Improvement
CMS estimates this to have $3 billion in 10-year savings.
Learn more about how AArete is working with Payers across the country to address quality service challenges
Health Equity Index (HEI) Rewards Replacing Existing Reward Factor
Starting Star Rating Year 2027, CMS is proposing utilizing an HEI Reward factor, incentivizing plans to improve member’s social risk factors.
CMS estimates this to have $5 billion in 10-year savings.
Guardrails Lifted for non-CAHPS Measures
Previously inserted to increase the predictability and stability of cut-points, the “trade-off is the inability to keep pace with any unanticipated changes in industry performance.” This will largely impact 2 and 3 Star Cut Points; 4 and 5 Star cut points have become more predictable. With the new Tukey outlier deletion methodology, the cut-points are expected to be more predictable.
Source: https://public-inspection.federalregister.gov/2022-26956.pdf
Need a customized solution to address your Star Rating? Get in touch with Alex and our Quality Services team by completing the form below
Learn more about AArete’s Quality Services solutions