Actionable Remediation Plan for CPS Optimization Created for Managed Care Organization
This is an AArete Healthcare Payer insight
Situation
A Managed Care Organization (MCO) wanted to identify Claims Payment System (CPS) optimization opportunities across three primary areas: configuration, EDI, and custom edits. They had a goal to optimize system set up and performance prior to the migration and scaling of products/members to a new self-hosted version of the platform from membership on both existing and legacy systems.
Approach
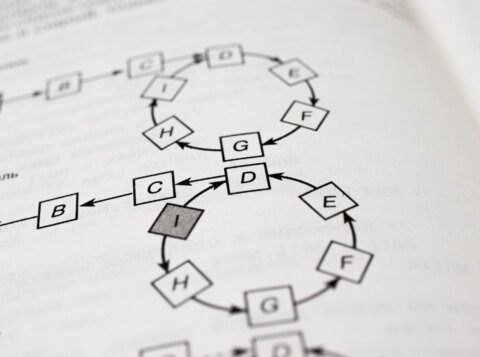
Working directly with operational teams to understand the current state pain points and future state requirements, multiple active areas were identified.
These included:
- Stakeholder interviews
- Collaborative bi-weekly stakeholder meetings
- Design of a custom database for detailed analysis and quantified opportunity identification
- Error reporting and resolution with CPS vendors
- Documented findings and recommendations on improving infrastructure to enable scalability
Results
AArete identified 45 actionable recommendations for implementation prior to client migration and collaborated with the MCO directly to develop a sequenced remediation plan.
The MCO utilized AArete’s assessment output to optimize their CPS setup for migration, including improvements to processing time, reduction in manual processes, improved payment accuracy, enhanced provider experience, and resolution of regulatory compliance challenges.
Learn more about AArete’s Digital & Technology solutions