Pharmacy Benefit Manager (PBM) Data Load Re-Engineering
This is an AArete Healthcare Payer Insight
Situation:
AArete’s client, a leading, multi-state commercial healthcare payer was transitioning to a new Pharmacy Benefits Manager (PBM) and realized the incoming PBM data could not readily be integrated into its Analytics Data Warehouse (ADW). This was due to the new PBM using an updated NCPDP standard, which had newer fields and attributes for better analysis of Pharmacy Claims. In addition, different carriers associated with the new PBM required carrier-specific logic instead of a more generic logic implemented for all of the carriers.
The client engaged AArete to integrate incoming PBM data into the client’s existing workflows while minimizing disruption to business processes and service to members.
Approach
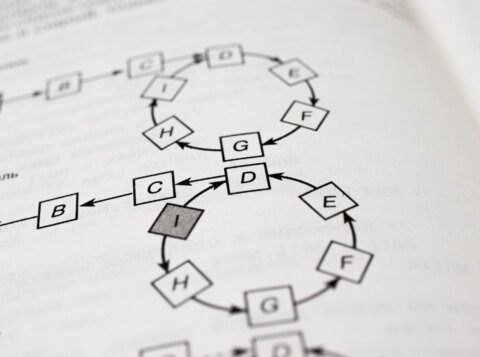
AArete reviewed the current ETL process (extract, transform, and load) from the incumbent PBM, and identified gaps to address when onboarding the new PBM data.
Data included (a sample):
- Claims
- Prior authorization
- Rebates
- IPD analytics
Using existing client-defined standards, we resolved the gaps to seamlessly integrate the new data. To improve reporting capabilities, we created a centralized view for all pharmacy data for various PBMs to equip the client with actionable insights.
Results
- Aligned and integrated incoming PBM data into existing workflows
- Created centralized view for all pharmacy data
- Minimized disruption to business and member service
Learn more about AArete’s Data & Analytics solutions