Right-Sizing the OR Block Schedule: A Powerful Avenue to Growth and Efficiency

A significant reduction in surgeries is among the many byproducts of the COVID-19 pandemic that have impacted the US healthcare system. Millions of elective surgeries were postponed in 2020 and early 2021, as hospital systems opted not to perform nonemergent procedures to preserve resources and patients chose to delay surgeries for fear of exposure to the virus. The OR is the single largest revenue generator for most hospitals, with surgical procedures and recovery/follow-up accounting for 60-70% of total revenue. Hospital systems saw patient volume decreases of as much as 70% for surgery during the pandemic, with many health systems reporting revenue reductions of more than 40% over that time. It is estimated that hospitals lost a total of $22.3 billion for unperformed surgical procedures, and that it will take the typical hospital one to two years to return to previous OR utilization levels.
This unprecedented drop in revenue happened during a time when hospital costs spiked due to factors like increased paid sick leave for healthcare workers, the need to purchase additional personal protective equipment that was selling at a premium due to demand, and the universal price spike for goods and services from a severely stressed supply chain. Now, as people increasingly return to the healthcare system, demand for those delayed elective surgeries is increasing, as 99% of the procedures that were delayed are expected to be rescheduled. Surely some of these losses will be readily recouped through surgical growth.
Or will they? OR scheduling is a challenge even in the best of times due to a range of factors that include hospital politics and resource constraints. Now, with more demand than ever, surgical services departments are struggling to balance block time allocation, surgeon access, surgical growth, and OR efficiency. On top of that, surgical throughput is being hampered by a number of factors, including a scarcity of patient rooms, worker shortages, and OR capacity.
But because an OR’s most valuable resource is ultimately the finite number of hours in a day, effective management of this precious time is of the utmost importance. Too often, perception of time availability does not match reality. Many ORs are over-blocked, with surgeons feeling like they have limited access while actual OR utilization is low due to inefficient scheduling. Considering that OR time costs from $35-$50 per minute, time is literally money.
Accurate surgical case forecasting is required to effectively meet demand and seize the current opportunities for surgical growth. Hospitals need to focus on managing resources and predicting how many ORs should be blocked not just on a given day, but also over the coming quarter and year.
The Block Allocation Struggle
Block allocation is highly complicated due to a host of competing stakeholder priorities. Surgeons want OR access when they want it — and expect their demands to be met. Anesthesiologists prefer to work a fairly traditional daytime work schedule, and otherwise only in emergency situations. Nurses want the rooms full during their twelve-hour shifts, but they also want their meal and break times. With outpatient procedures increasingly outnumbering inpatient ones, patients hope for their surgeries to take place during times that are convenient for themselves and their loved ones in the waiting room. All the while, hospital administrators dream of some sort of perioperative services paradise in which all their operating theaters run 24 hours a day while steering clear of costly overtime.
Administrators strive to balance the surgical staff’s need for access, safety, and quality with the need for efficiency and productivity. But even with e-scheduling tools, the desired balance is rarely achieved, in part because it is neither data-driven nor transparent. Plain and simple, there is a very clear need for a better block-need forecasting process that allows for growth in revenue-generating surgical services as well as cost savings through more effective OR utilization.
Right-Sizing the OR Blocks
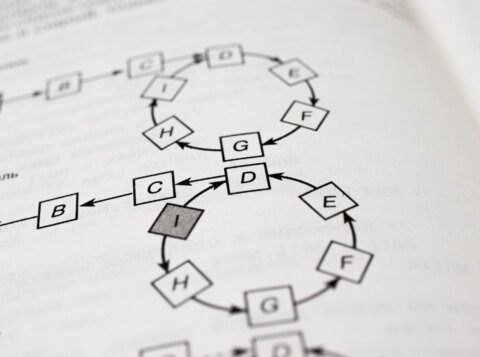
Based on historic practice patterns and a few assumptions, the block needs for each surgeon by day of week can typically be predicted. But the challenge around doing so lies in extracting accurate data from the electronic medical record system to manage clear block utilization expectations. By leveraging a data-driven approach centered on an analysis of surgical minutes used, OR turnaround time, and expected utilization, each surgeon’s block need can be determined.
Buy-in by the surgical staff is critical to making this process a success. Once the initial forecasts are developed, the data should be shared with surgeons so they can request blocks based on their individual forecasts. Because these forecasts are based on actual surgical minutes rather than a block utilization percentage calculation that the surgeon might not agree with, they provide a neutral, apolitical mechanism to optimize block time.
Once all surgeon block needs have been forecasted and block requests received, an ideal block schedule by day of week and week of the month can be developed. One thing to bear in mind is that since patients typically meet their deductibles by the fourth quarter of the year, surgical volumes can significantly fluctuate throughout the year. Because of this fluctuation, in many cases it is better to build the schedule based on quarterly practice patterns rather than annual utilization.
As with many transformation efforts, the challenge around obtaining, cleansing, and putting data to work can appear intimidating at first blush. Outside data experts can and should be engaged to assist with this challenge or even to manage the entire block scheduling development process, allowing hospital system resources to concentrate on their core competencies.
Data Drives Success
Success in the block scheduling process hinges on having all relevant information available, which requires reliable data and transparent block expectations coupled with a governance structure to enforce the guidelines.
A multidisciplinary governance structure is needed to determine the block schedule expectations, disseminate policies, and ensure compliance. It is up to the governing body to decide which assumptions to factor into the model, including block length minimum, block utilization thresholds, and growth factors. Typically, a subcommittee evaluates the forecasts and requests, considers the real-world constraints (e.g., how many ORs there are, which ones have highly specialized equipment like robotic surgical assistants), and builds a new schedule.
After the block schedule has been redesigned, it is critical to ensure that:
- Hospital administration empowers the governance committee to make all block schedule decisions.
- Block utilization reports are shared regularly (at least once per quarter) with surgeons.
- Rules around block utilization are impartially enforced by the governance committee and supported by the administration.
- Alterations to the schedule are made according to policy and the guidelines are adhered to in a fair and transparent manner.
A systematic, data-driven approach to block forecasting has been shown to have positive effects on OR culture and efficiency, which helps to improve surgeon satisfaction and increase case volume. As hospitals look to catch up with the backlog of elective procedures that they were unable to perform during the pandemic, maximizing OR utilization is critical to recouping lost revenues and ensuring efficiency to control costs.