The Hospital of the Future: Balancing Risk, Revenue in Post-Pandemic World

Healthcare providers have increasingly entered into value-based contracts with payers in recent years because they offer the opportunity to increase revenue-the primary driver of change for any business.
Healthcare providers have increasingly entered into value-based contracts with payers in recent years because they offer the opportunity to increase revenue-the primary driver of change for any business. Since these contracts are centered on quality and performance metrics rather than traditional fee-for-service care, they represent a substantial shift in the provider payment model that requires providers to significantly change their organizations’ behavior and culture. But providers are willing to accept these contracts because they offer enough financial incentives to justify the increased financial risk.
For years these contracts were, by and large, upside only and did not include any downside risk to providers. They give providers the opportunity to increase revenue slightly by reaching established metrics without facing downside risk for falling short of the goals. The COVID-19 pandemic, however, has altered this risk calculation and left many healthcare systems short on cash.
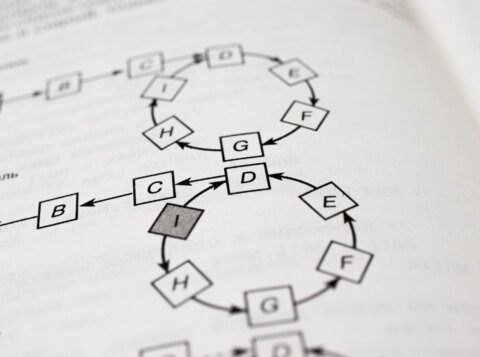
Although over half of all U.S. provider revenue is in a value-based payment model, typically only a small percentage of a provider’s revenue (2% to 8%) is at risk under these contracts. Because the amount of risk is the real driver of change and providers only have a small amount of revenue at risk, they have not yet hit the tipping point where value-based care creates the need for meaningful change across the country. However, the recent pause to have higher margin services like elective surgeries performed during the pandemic has caused cash flow challenges for providers that can be addressed through value-based contracts. Even as most states are resuming elective surgeries there has been a slow response by patients to opt for these services indicating the effects on provider revenue may linger for quite a while.
Providers that have been succeeding with their current deals and can see the potential to boost revenue are starting to move farther along the value-based spectrum. Others will soon follow. Increased adoption of this payment model, however, will shift more risk to providers, making them more accountable for cost. It will likely force them to take steps to cut additional costs in order to better manage risk, which will hasten the movement toward the hospital of the future.
Tomorrow’s Hospital
The hospital of the future’s inpatient setting will more than likely be much smaller and have fewer beds than today’s facilities for the simple reason that as providers take on more risk, they will need to shed cost and find ways to eliminate overutilization of services. Under this prognostication, this smaller hospital may be designed primarily for acute care services, such as surgery, neonatology, intensive care and the ER. Most chronic care and other services provided in today’s large facilities may be delivered downstream at lower-cost, more efficient outpatient and long-term care facilities. While some of these facilities will be independent, it is expected that providers will look to vertically integrate many of them into their own businesses by establishing new locations and acquiring others.
To further mitigate risk, cut cost, and increase revenue, providers will likely shift as many services as possible completely out of hospitals and downstream facilities-and into members’ homes. This shift should be enabled in part by advancements in technology that soon will make it possible for almost half of all medical services to be performed at home rather than in an inpatient or outpatient setting. Without leaving their homes, it’s expected members will regularly visit their doctors via telemedicine appointments from their phones, tablets or computers. When ultra-fast 5G wireless technology becomes available across the country, blood, glucose and other diagnostic tests may routinely be conducted over the internet, with the results in turn delivered electronically.
As providers build tomorrow’s small hospitals and shift services downstream to less costly locations, the shift towards preventative care is likely to increase rapidly. This approach will encourage increased member engagement in their own healthcare and greater physician collaboration to more efficiently address a member’s various needs.
When will the hospital of the future dominate the healthcare landscape? Prior to the COVID-19 pandemic, a 10- to 20-year time horizon seemed likely; this could well accelerate if providers and payers come to better appreciate the mutual benefits of employing value-based contracts in order to make more consistent payments through risk-based payment models. The timeframe depends on many factors that include regulatory, organizational, technological, and cultural changes, which we are slowing moving towards. One day soon we will hit a tipping point where the industry rewards quality of care over volume of services and organizations become more profitable as a result.
Without a doubt, making these sorts of major changes will prove challenging for many payers and providers. But doing so is the only way to create the hospital of the future-the keystone to success for providers in the 21st Century.
This article was originally published in Managed Healthcare Executive.