Addressing the Crisis: The Cause and Effect of Healthcare Provider Staff Shortages
This is an AArete Healthcare Provider insight
The healthcare industry has long been plagued by staff shortages, but in recent years, the problem has grown increasingly severe. As the demand for healthcare services continues to rise, organizations are struggling to find and retain qualified healthcare professionals to meet patient needs. This healthcare workforce shortage affects not only the quality of patient care but also the financial viability of healthcare organizations.
The Causes of Staff Shortages in Healthcare
One notable reason for the current shortage of healthcare staff is the change in morale following the COVID-19 pandemic. Healthcare professionals have worked tirelessly on the front lines of the pandemic, putting their own health and safety at risk. Many have experienced burnout and fatigue due to the overwhelming demand for their services, with some workers leaving the industry due to fear of exposure to the virus, or because they had contracted the virus and are unable to work. The loss of experienced nursing staff, as well as other healthcare workers, has put an additional strain on an already overburdened system.
What is the main cause of the nursing shortage?
Another factor contributing to the shortage of healthcare providers is poor compensation and treatment. Healthcare workers are often underpaid and overworked, leading to low job satisfaction and high turnover rates. This is particularly true for professions such as nursing, which is known for its high levels of burnout and turnover. According to the American Nurses Foundation and American Nurse Association, a survey of over 12,000 nurses demonstrated that “52% of nurses are considering leaving their current position due primarily to insufficient staffing, work negatively affecting health and well-being, and inability to deliver quality care. In addition, 60% of acute care nurses report feeling burnt out, and 75% report feeling stressed, frustrated, and exhausted.” A major overhaul is needed in retaining top talent, and improving compensation and working conditions is just the beginning when it comes to solving the nursing shortage.
It is important to note that an increased acuity of patients has contributed to the shortages in the healthcare workforce. Advances in medical technology and treatments have led to a growing population of older and sicker patients who require more complex care. This has put a strain on healthcare resources, leading to longer wait times for appointments and longer hospital stays for patients. Put simply, the increased demand for healthcare services has led to a greater need for nursing staff and healthcare workers, but the supply has not kept up with the demand. As a result, healthcare organizations are struggling to find enough qualified providers to meet patient needs.
What are some factors that can cause a healthcare staff shortage?
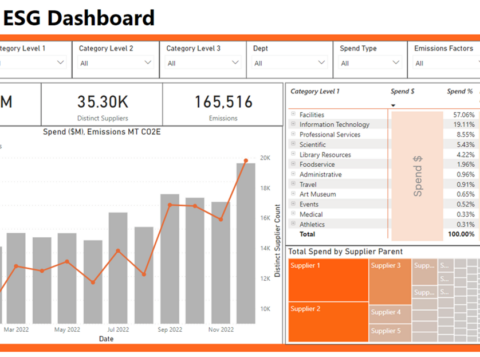
In the past five years, there’s been a 105% average hospital workforce turnover rate with voluntary terminations accounting for 94.7% of them, according to the 2023 NSI National Health Care Retention & RN Staffing Report, but healthcare provider staffing shortages can vary widely depending on the type of provider. For instance, there is currently a shortage of mid-level providers and allied healthcare professionals such as physician assistants, nurse practitioners, and certified registered nurse anesthetists. An increased demand for healthcare services, as well as the aging population and the retirement of many experienced practitioners, attribute to some of these shortages. In contrast, voluntary terminations have caused shortages in other areas, such as nursing and allied health technicians, due to personal reasons, career advancement, and relocation.
Location is also a major factor in the shortage of healthcare workers. Inpatient and outpatient settings may have different staffing needs, as may imaging centers and surgical centers. For example, inpatient facilities may require more nurses and physicians to manage complex medical conditions, while outpatient facilities may require more allied healthcare professionals to manage a higher volume of patients. Additionally, certain specialties may require specific staffing levels. For example, a perioperative setting may require more surgical technicians, while an imaging center may require more radiologic technologists.
Additionally, rural areas may experience more severe shortages than urban areas, as there may be fewer healthcare facilities and a smaller pool of qualified providers. Certain regions may also have a higher demand for primary care providers due to an aging population, while other regions may have a greater need for specialists in fields such as cardiology or oncology.
The type of hospital can also play a critical role in staffing. Academic medical centers may face unique challenges in recruiting and retaining providers due to their emphasis on research and education. Meanwhile, standalone hospitals may struggle to compete with larger hospital systems that can offer higher salaries and benefits packages. In contrast, community hospitals may be more attractive to providers who value a more personal approach to patient care.
Needless to say, the multitude of factors contributing to staffing shortages are complex. So, is there anything healthcare organizations can do about it?
How can we fix the healthcare staffing shortage?
According to National Academy for State Health Policy, “The lack of workers has become so dire that at least 20 governors this year directly addressed the situation in their state of the state speeches, proposing a range of policy fixes.” It’s also worth noting that today, only 48.8% of hospitals track the cost of turnover rate; an alarming, despite the average cost of turnover for a staff RN being $52,350.
Policy changes are just the beginning. Given elevated RN turnover, the average hospital lost $8.55M in 2022. This means that hospitals could save $380,600 per year for each percentage of change in RN turnover. Invest in healthcare professionals and develop retention strategies, such as expanding educational opportunities and offering scholarships and/or loan forgiveness programs, or optimizing your scheduling for work flexibilities (i.e. remote or part-time) to retain healthcare providers. A simpler method for retention can include forming a committee within health organizations to solely focus on improving working conditions and increasing compensation for healthcare providers to attract and preserve talented individuals.
With the recent shift toward virtual settings, implementing telemedicine and other technology-based solutions can help to maximize the impact of existing staff and reduce the need for additional personnel. This, combined with collaborating with staffing agencies and partnering with other healthcare organizations to share resources and expertise, can help to address staffing shortages. By implementing a combination of these solutions, healthcare organizations can work to alleviate staffing shortages and provide high-quality care to patients while effectively managing costs.
Learn more about AArete’s Profitability Improvement solutions