7 Considerations for Health System CFOs

Health systems are struggling as a result of the reduced activity of elective procedures, the loss of health coverage for many employees, and the resultant drop in billings. According to this article, there are seven approaches recommended for immediate consideration to increase revenues and stanch losses.
The COVID-19 pandemic is wreaking havoc on every industry, and healthcare is no exception. In many states, elective procedures—the main driver of hospital profitability—were not allowed for several months, and some providers continue to limit them. Many people, especially those with comorbid conditions, have anxiety about coming into hospitals and doctors’ offices and are opting instead for telehealth visits, for which providers have had difficulty getting full reimbursement.
More than 5 million Americans who lost their employer-provided health plans are currently uninsured, keeping many of them outside of the healthcare system for anything outside of emergencies.
Needless to say, health systems are struggling as a result of this reduced activity and the resultant drop in billings. What can be done to increase revenues and stanch losses? Based on our industry experience and conversations with a number of healthcare executives, we’ve determined seven approaches that we can recommend for immediate consideration.
1. Invest in outreach programs to reduce patient anxiety. Too many patients with chronic conditions have gone months without the in-person care and lab work that they need to properly manage their conditions and avoid complications. Targeted outreach to these patients is essential to help them avoid adverse events. Beyond that, those who are past due for their diagnostic exams or follow-up visits for a range of conditions, and others who have delayed care during the pandemic should be contacted and educated on the best approach to keep them safe and maintain their health. As with any other intervention, it is important to identify the patients most in need, and then exert the appropriate effort to get them in the door.
2. Evaluate all opportunities for strategic cost reduction. We absolutely caution against any further reductions in workforce, but otherwise believe that all areas are fair game for cost reduction right now. All vendor contracts that were signed prior to the pandemic should be reevaluated, as they were negotiated and agreed to based on volume assumptions and other considerations that no longer reflect reality. Vendors are understandably concerned that they may lose some accounts, so this is a prime opportunity to discuss renegotiating terms. Those health systems that act first will achieve the best results from this practice, as the race is on to reduce costs.
3. Examine payer relationships and contracts. Like your vendor contracts, your payer contracts were agreed to under assumptions of volume, visits, and procedure counts that are no longer relevant. It is critical that you examine them and approach payers with data-driven approaches to optimizing contracts, revenue and reimbursements.
4. Seek opportunities to leverage technology in shared services. A wide range of increasingly cost-effective technologies, such as robotic process automation and predictive modeling, has shown real value as a way to supplement full-time workforce (FTE)-heavy functions like IT service desk, Human Resources, and Revenue Cycle. In many cases, this technology is more efficient, scalable, and less prone to error than the current approach, and it also frees up those resources to take on more high-value, stimulating work, where human judgment and experience are essential.
5. Maximize new or existing value-based contracts to reflect the low patient volumes. The current low volume of services being provided to patients would have benefitted any providers that aggressively pursued value-based contracts prior to the pandemic. While that opportunity may have passed, it is not too late to explore new models and receive revenue-sharing benefits from health plans willing to negotiate them. A specialized, skilled, third-party advisor can help to evaluate these opportunities and facilitate the creation and management of these new contracts.
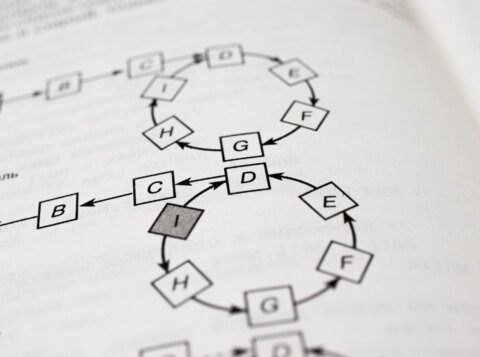
6. Use data and predictive models to transform entrenched practices. There are many decades-old practices in healthcare that are ripe for reform via data and predictive models, and the COVID pause has provided an ideal moment to make these changes. They might include areas that have a high impact on revenue and cost, such as procedure scheduling and nurse staffing models. Too often, surgery schedules are created without prioritizing profitability, and can’t predict rate-limiting resources. Similarly, nurse staffing tends to rely on benchmarks and a subjective perception of history, which can lead to the considerable use of overtime and agency nurses. Leveraging predictive models to replace these inertial approaches can reduce these premium costs and better predict the necessary nurse staffing to achieve optimal clinical as well as financial outcomes.
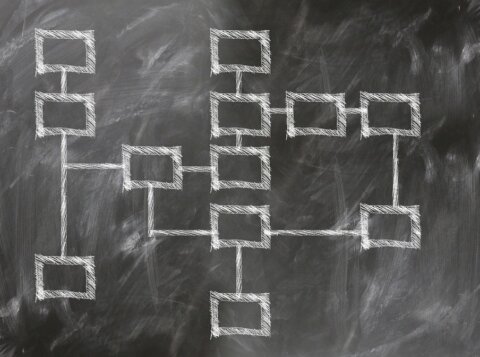
7. Evaluate the project pipeline to focus on those with a clear business case. Often the decision-making process for project funding within a health system can be siloed, and it can be challenging to gauge which projects are most aligned with organizational value. A strong governance process that prioritizes projects according to the underlying business case can drive the appropriate investments, at a time where every expenditure of resources is critical. Evaluating the project pipeline and measuring each project, whether proposed or in-flight, in terms of its relative organizational value can likely free up capital, operational, and FTE expense. Baking that value index into future approvals allows for appropriate spend approval and prioritization.
These are undoubtedly among the toughest times of your career. But actions like targeted patient outreach, strategic cost reduction, an improved approach to capital projects, optimized contracting, and smarter use of data and technology can not only help your system weather the current storm but position you for new successes when economic conditions improve.
This article was originally published in Managed Healthcare Executive.