Medicaid Managed Care Organization Reduces Inaccurate Payments by $2.20 PMPM by Engaging AArete
Situation
A local Managed Care Organization (MCO) was inappropriately reimbursing providers for unauthorized and non-covered services. The MCO approached AArete to conduct a comprehensive system configuration review of benefits and prior authorization.
Approach
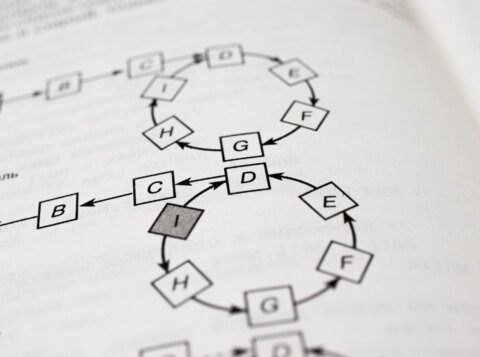
AArete documented the state and MCO’s policies and compared it to the prior authorization setup and benefits configuration setup. For all discrepancies between policy and configuration, AArete quantified the applicable recoupment, prospective savings, and any key provider insights associated with the configuration fix. All recommended adjustments to configuration were documented and discussed with the MCO, including solutions to minimize provider abrasion. AArete also worked with the MCO to implement an easy-to-adopt process to track changes to configuration.
Results
The MCO reduced their inaccurate reimbursements by an estimated $2.20 PMPM for the first year after engaging AArete. Communications scripted by AArete helped to keep provider noise at a minimum during the recoupment process. The MCO adopted AArete’s recommended process to track benefit and prior authorization policies, reducing the amount of time required by the department to maintain proper configuration.