AArete Fraud, Waste and Abuse (FWA): Identification of Missing Rate Codes
At A Glance
Situation:
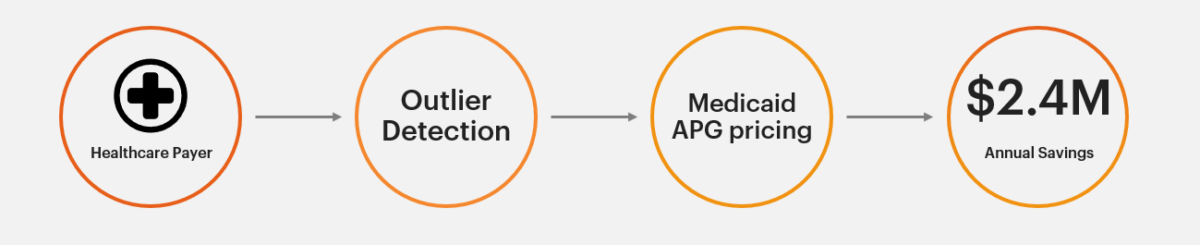
A large Managed Care Organization engaged AArete to provide payment integrity cost-reduction support by reviewing their medical claims data, payment policies, state reimbursement guidelines, and provider contracts.
Approach
AArete ran proprietary outlier detection models on 24 months of claims data, which led to a focus on Medicaid outpatient claims utilizing APG (Ambulatory Patient Group) reimbursement methodologies.
Reimbursement methodologies were reviewed against provider contracts, state guidance, and existing auto-adjudication logic.
Results
AArete detected and saved our health plan client $2.4M annually by identifying contract adherence and APG reimbursement gaps with two key network facilities. The client implemented a system fix for proper ongoing claims payment.