4 Tactics to Address Uptick in CARES-Related Billing and Other Claims Denials

With the uptick in claims denials, which have increased sharply due to CARES-related provisions, the onus is on providers to directly address a problem that’s only going to get worse as we continue to work our way through the COVID-19 pandemic. Recommended is a 4-pronged approach for providers to address this.
With the uptick in claims denials, which have increased sharply due to CARES-related provisions, the onus is on providers to directly address a problem that’s only going to get worse as we continue to work our way through the COVID-19 pandemic. We recommend a 4-pronged approach for providers to address this: first, mitigate; second, analyze; third, predict and fourth, prevent.
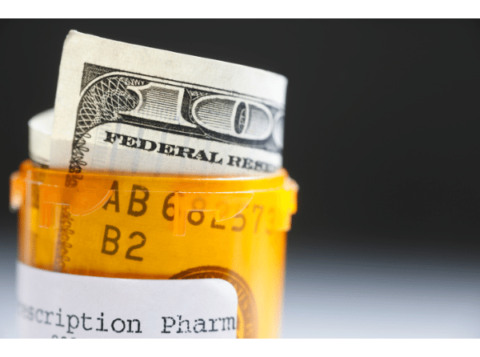
As payment models continue to change and provider revenues shrink—putting margins under even more extreme pressure—healthcare providers can no longer afford the risk to their bottom lines caused by having claims denied. They need to do everything in their power to receive all the money owed to them—and that includes better reducing the incidences ofdenial so they get paid for all the claims they submit. According to Change Healthcare, claim denials amounted to $262 billion for U.S. healthcare providers in 2017 alone.
Every health system has in place a denial management team that operationally oversees the appeals process for denials. But these teams typically are charged with shuffling denials through the lengthy process without solving the underlying problems that cause them. They review each denial on a claim-by-claim basis, as if it were unrelated to similar past or current denials—and certainly without trying to predict, and avoid, similar denials in the future. Treating denials on a production line, without identifying commonalities and trends, leaves providers in a constant retrospective battle against denials. By understanding and anticipating the reason for denial, the claim can be submitted correctly from the onset, preventing the denial before it even happens.
By grouping claims denials into common themes—identifying root causes in either operations, coding/documentation, or other process breakdowns throughout the organization—healthcare organizations can begin to identify ways to catch these issues pre-bill. This proactive approach would enable them to use their existing technology and massive amounts of data to identify and correct potentially denied claims before they ever land in the appeals process. Overall, it would make avoiding denials more efficient and less wasteful of time, resources, and revenue. Becker’s identifies that it costs healthcare organizations an average of $118 per claim to work a denial – applying this statistic to your organization’s denial volume quickly identifies a financial reward to resolving increasing denial trends.
But most providers either are either unaware of this approach or do not know how to employ it to take advantage of the technology and data they have at their disposal. So they wind up using only a small percentage of their potential for mitigating denials. This unused potential is like owning a Ferrari but leaving it idling in the garage because the owner does not have a driver’s license.
Predictive Analytics Mitigate, Analyze, Predict and Prevent Claims Denials
The predictive analytics approach to avoiding denials is radically different from relying on a team of legal, contract, billing/coding, and denial experts to go back over the process to see what went wrong and led to a claim being denied. This new approach seeks to proactively fix any problem with a claim before it goes out the door, thereby eliminating denials and the need to rehash the process they initiate. In doing so, it drives higher margins by stopping any revenue loss for a particular case. More importantly, it also stops revenue loss caused by poor performance in risk-based arrangements, inappropriate quality reporting because of misrepresentation of case acuity, and unsatisfied patients who shop their healthcare needs to other providers.
Three key capabilities inform the predictive analytics approach to avoiding denials:
- Understanding how payers view the claims they deny, their reasons for denying the claims, how they interpret contracts with providers, and how they then turn this information into denial reason codes.
- Developing insights from this understanding and from the data currently available in the provider’s database.
- Using these insights with the existing technology to identify the probability of a denial, in some cases before the patient has even been discharged.
What does it take to get this right? Experience working with both payers and providers and a high level of comfort working with data and putting that data through the mill of predictive analytics.
A Simple Solution
Although this solution is simple for the provider, it relies on advances in predictive analytics to identify the link between claims data, denials data, and predictive modeling software to help detect the probability of a denial. Drilling into the details of the claim at the procedure code level will yield valuable insight toward the underlying issues and potential root causes of denials. Using this insight to build work-queues and other pre-bill operational flags takes the denials process from a retrospective re-bill to a more predictive stop, assess, and fix prior to billing.
The historical data may show, for example, that the cardiology unit has a higher volume of denials than other departments. The program then would dive into the data to pinpoint the source of the problem by taking steps such as the following:
- Identifying the specific doctor who typically receives a denial when his patients discharge under MS-DRG 305 (Hypertension without MCC) and have a length of stay above three days.
- Identifying the particular DRG/doctor pairing as having a higher risk for denial problems.
- Comparing the insight from this data to payer contractual elements, operational elements, and other factors that could lead to length-of-stay issues.
- Creating a process flag in the provider’s existing technology to notify a care manager to review the care plan and identify any issues in coding or billing whenever a patient is admitted under working DRG 305.
This proactive approach—coupling data insights, delivering experts where required via process flags, and proactively mitigating problems—helps drive the predictive denials mitigation engine.
Healthcare providers have an overwhelming quantity of data at their fingertips. Now they need to start harnessing the power of the insights available in this data and using it with their existing technology to take a predictive analytics approach to mitigating denials before claims are presented to payers. This approach, which eliminates wasted, costly steps of the current labor-intensive process, provides a way for providers to improve revenues, appropriately utilize resources, and ultimately increase margins in today’s tightening healthcare economy.
This article was originally published in Managed Healthcare Executive.