Smarter Healthcare Accumulator Management for Stronger Operations
Overcoming the Operational Burden of Traditional Healthcare Accumulator Management
Accumulator management remains a critical, yet often problematic, component of healthcare claims processing for payer organizations. Accumulators in healthcare—such as deductibles, out-of-pocket maximums, and benefit limits—are central to enforcing plan design, controlling costs, and informing both payers and members about benefit utilization.
However, many health plans continue to struggle with fragmented accumulator management systems that hinder operational efficiency, create member dissatisfaction, and pose compliance risks.
Why Accumulators in Healthcare Create Persistent Challenges for Healthcare Payers
As benefit design becomes more complex and member expectations continue to rise, many payer organizations struggle to manage accumulators effectively. To focus on a fix, it’s worth defining the key health plan challenges worth narrowing in on, including:
- Fragmentation of data across disparate systems
ERP accumulator integration is often missing, and accumulator information for medical, pharmacy, dental, and vision benefits is frequently maintained in separate platforms. This makes it difficult to aggregate and reconcile member benefit usage—particularly for integrated accumulators or complex family plans. As a result, claims may be adjudicated using outdated or incomplete accumulator values, leading to inaccurate payments, denials, or rework. These delays and discrepancies in updating accumulators can erode trust with both members and providers.
- A lack of real-time processing capabilities
When accumulator balances are not updated instantaneously during adjudication, it opens the door for benefit over-utilization or under-utilization. This latency often requires claims examiners to manually intervene, increasing administrative burden and introducing the potential for human error.
- Audit and compliance challenges
When accumulator systems lack sufficient traceability and transaction history, it poses a greater risk for the health plan.
- The complexity of modern benefit design
Plans frequently incorporate tiered structures, service-specific limits, integrated medical and pharmacy deductibles, and family-level accumulators. Traditional systems often lack the flexibility to support these structures, resulting in inefficient workarounds or system limitations that cause payment inaccuracies and policy enforcement issues.
From the member’s perspective, lack of transparency into real-time benefit utilization is an ongoing pain point.
From Fragmented Systems to ERP Accumulator Integration
When accumulator balances are not updated instantaneously during adjudication, it opens the door for benefit over-utilization or under-utilization. This latency often requires claims examiners to manually intervene, increasing administrative burden and introducing the potential for human error.
An integrated ERP accumulator solution closes these gaps by unifying data sources, streamlining workflows, and ensuring accurate real-time benefit tracking across all plan types.
Together, they ensure that pricing, benefit design, and accumulators are aligned with enterprise financial data, enabling accurate adjudication, seamless reconciliation, and transparent reporting across the healthcare ecosystem.
Choosing the Right Accumulator Management System
Choosing the right healthcare accumulator management system solution is essential to enabling a more effective and efficient claims processing system.
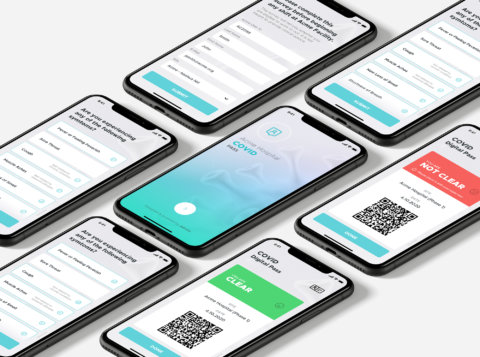
For example, Pegasystems’ Smart Claims Engine (SCE) includes a robust accumulator management system component, offering advanced capabilities to automate and streamline benefit limit tracking across healthcare claims lifecycle.

This solution supports real-time processing, accurate accumulator tracking, and comprehensive integration capabilities—empowering payers to maintain precise control over member benefit utilization while improving the speed and accuracy of claims adjudication
How Do 340B Accumulators Work in Claims Processing?
The 340B program creates unique challenges in claims processing. Covered entities purchase drugs at steep discounts, while health plans reimburse at standard rates. To prevent members from reaching out-of-pocket maximums more quickly due to these discounted drugs, many payers apply 340B accumulator rules during adjudication. This requires the claims system to detect 340B claims, apply cost-share logic, and update benefit ledgers with precision.
Pega’s Accumulator Management offers an ideal platform for handling these complexities. With its rules-driven engine, payers can:
- Configure accumulator policies that exclude 340B drugs from advancing member deductibles or out-of-pocket maximums.
- Integrate across claims, pharmacy, and UM systems to ensure consistent handling of 340B indicators and modifiers.
- Provide transparency through audit trails and dashboards, giving payers insight into how 340B claims impact overall cost-share tracking.
- Adapt quickly as regulations or contract terms change, without requiring hard-coded changes in the core claims system.
Smarter Accumulator Tracking with AArete Healthcare + Pega
AArete partners with Pegasystems to help healthcare payers implement smarter, scalable accumulator management software. With Doczy.ai™ and AArete’s healthcare consulting expertise, payers gain advanced AI-powered analytics, workflow automation, and compliance assurance across all accumulator types.
Benefits of Modern Healthcare Accumulator Solutions
Implementing advanced accumulator management delivers measurable benefits across accuracy, efficiency, compliance, and member satisfaction:
- Enhanced Accuracy – A modern healthcare accumulator solution reduces manual tracking errors, integrates ERP accumulators, and ensures real-time benefit transparency.
- Operational Efficiency – Automates repetitive tasks, accelerates claims adjudication, and reduces administrative overhead.
- Regulatory Compliance – Delivers detailed audit logs and transparent tracking aligned with federal and state requirements.
- Improved Member Experience – Real-time tracking ensures members have visibility into their benefit usage, supporting financial planning and minimizing disputes.
- Holistic Integration – Connects internal systems and external vendors to enable cross-benefit reconciliation and maintain ecosystem-wide accuracy.
Why Partner with AArete Healthcare for Accumulator Management
As the complexity of healthcare benefit design continues to evolve, payer organizations must adopt advanced technologies to manage accumulators with precision.
With 17 years of healthcare consulting experience, AArete Healthcare delivers measurable results in accumulator management. From advising payers on how 340B accumulators work to implementing scalable accumulator management systems, AArete ensures operational precision and stronger payer-provider relationships.
As an authorized Pega partner, AArete aligns technology with payer strategy, accelerating time-to-value while minimizing disruption.
Below is an outline of our key accumulator management features and benefits of the Pega Smart Claims Engine that we find especially valuable to highlight when evaluating enterprise smart claims engine (SCE) solutions—and when prioritizing implementation efforts, taking into account the following:
Functional Capabilities
- Comprehensive Accumulator Tracking: Manages a wide range of accumulator types, including deductibles, out-of-pocket maximums, and benefit limits, ensuring precise and up-to-date tracking of member benefit utilization.
- Seamless Integration with Healthcare Applications: Provides APIs that enable integration with core healthcare platforms and administrative systems to efficiently create, retrieve, and update accumulator data.
- Manual Management Capabilities: Enables authorized users to view, create, update, or delete accumulators and transactional details, allowing flexible exception handling and manual adjustments when needed.
- Detailed Historical Records: Maintains a full history of all actions performed on accumulators, offering transparency and support for audit readiness and regulatory compliance.
- Discrete Workflows: Accumulator management functions are supported by discrete, primarily automated workflows that allow retrieval, updates, deletions, and creation of new accumulator records. These processes are typically executed during claims auto-adjudication and integrate directly with the health plan’s claims engine or equivalent systems.
Accumulator Types Tracked
- Financial Accumulators:
- Individual deductibles
- Family deductibles
- Individual out-of-pocket maximums
- Benefit Limit Accumulators:
- Number of visits
- Units of service performed
- Number of days
- Authorization Accumulators:
- Tracks service utilization against pre-determined authorization limits, in financial or usage units (e.g., visits, units, days).
Implementing advanced accumulator management within Pega Smart Claims Engine delivers measurable benefits across accuracy, efficiency, compliance, and member satisfaction—driving operational impact at every level of the organization.
Get in touch with one of our experts to learn more
Read more information on AArete’s Pega-powered consulting services.
Meet The Authors
Amir Pakfetrat
Senior Director
Jennifer Kanipe, RN, BSN
Subject Matter Expert
About Guest Author – Jennifer Kanipe, RN, BSN
Jennifer Kanipe is a healthcare strategist and registered nurse with over 25 years of experience across clinical care, healthcare technology, and payer operations. As a former Healthcare Domain Consultant at Pegasystems, she served as a subject matter expert in Utilization Management and Care Management, guiding national health plans through enterprise platform implementations and workflow optimization. Jennifer brings a unique blend of clinical insight and system strategy, specializing in aligning payer operations with smart technology solutions to drive accuracy, efficiency, and regulatory compliance.