Playbook: A Four-Part Approach to StrongerMember Journeys and Growth for Health Plans
The AArete Retention Approach: A 4-Step Frame-Work for Payers
Building better member relationships doesn’t happen overnight—it should be a multi-step and highly data-driven process. Healthcare payers must build a customized plan that scales to meet the goals of the business and members’ healthcare needs in the current regulatory landscape.
The following four-step framework is a proven approach to evaluate and enhance the member journey across every channel. These steps will help you assess your current state, improve member relations, and optimize engagement.
Keep the elements above in mind as you review the current member journey in-depth:
EVALUATE COMMUNICATION EFFECTIVENESS: Review your existing outreach strategy. Which channels do you use to reach customers, and are they effective? How many are digital versus traditional? Are you using costly and inefficient channels like static letters or outbound calls? Without personalization or timely delivery, these channels often fall flat. In one client case, static letters and calls were the primary outreach tools and more than 70% of those attempts were ignored.
Consider your current response rate based on both channel and content. If your communication approach isn’t meeting your members’ needs or expectations, then it’s not contributing to a stronger relationship or supporting retention.
ASSESS MEMBER EXPERIENCE: Don’t just wonder about what members go through when they interact with your MCO. Walk in their shoes—use the platforms and evaluate how easy it is to find information or resolve issues.
By now, you should have reviewed member data to identify when members most often leave. Zero in on those moments: Are there technology challenges that keep members from enrolling or renewing? Do they abandon the experience due to specific frustrations or lack of clarity? Once you’ve determined the root causes of churn, you can take steps to solve them and bolster the member journey.
CREATE DATA-DRIVEN SEGMENTS: Each member’s needs are unique, depending on where they live, their health conditions, their socioeconomic status, and many other factors. This makes personalization a major challenge, but these traits can also guide your strategy by helping you to create defined personas.
Leverage the data from sources we’ve already explored to create meaningful population segments based on demographics, SDOH, health conditions, and risk assessments. With these personas in mind, you can build and enhance targeted engagement journeys that match individual and collective needs.
IDENTIFY OPPORTUNITIES FOR IMPROVEMENT: Once you’ve found key problems in the member experience, you can work to resolve them. In places where members need more guidance or instruction, introduce new touchpoints via their preferred channels. Instead of only reacting when members reach out or express an issue, proactively offer information they might need later, or remind them of a resource that could enhance their journey.
Where and How to Identify Churn Risk:
We’ve covered the many reasons voluntary churn can occur. But predictors of these gaps are more subtle – hidden in your data. Common risks can include:
- Poor first-call resolution rates for basic member inquiries
- Lack of awareness of re-enrollment timing, revealed through surveys or high volume of churn at those times
- Weak engagement with communications due to generic or poorly timed messaging
- Limited awareness of included services
- Care management that overlooks SDOH factors, including economic challenges, location and transportation, or social limitations
Start by reviewing the member experience. Look for patterns in the behavior of members who have churned, and identify similar warning signs in current members. Isolate the problems driving churn, and develop a roadmap for proactive strategies.
Effective churn analytics can help you create a reporting framework that identifies areas for improvement, connects members to specific marketing tactics, and defines the ideal outcome for each interaction and the next best action for the member to take.
Using trackable predictors reflected in the data, aim to calculate the total percentage of your membership that is at risk and the apparent cause for each one. This will reveal the scope of churn risks, how much revenue is at risk, and how many members are in need of improved care management journeys.
CHANNELS TO OPTIMIZE FOR MEMBER RETENTION
To deepen member relationships, most MCOs must prioritize adding or enhancing touchpoints in a few core areas:
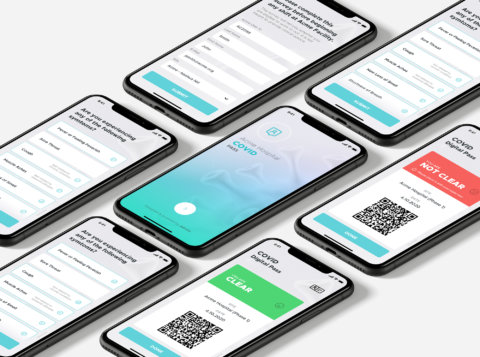
- Mobile strategy. Send SMS or mobile app push notifications to enrollees to provide important reminders or helpful information like appointment reminders, vaccine due dates, and prescription refills.
- Website and portals. Create streamlined pathways for electronic access to relevant member information. Make it easy for members to find Explanation of Benefits, new member packets, in-network providers, and benefits like gym memberships, rewards, and health assessments.
- Social media. Entice members to follow and engage through social channels to build a thriving community on Facebook, BlueSky, Instagram, and X. Share timely and value-added information, and create two-way Q&A interactions.
- Customer service. Deepen the support experience by ensuring easy access to call centers, chat engines, and customer service email portals where members can submit questions, feedback, and concerns. Go even further to build member rapport with proactive outreach and personalized care management services.
- Community partnerships. Partner with community-based organizations for educational events, housing needs, childcare, or food delivery for vulnerable members.
After uncovering common predictors of churn and ways to improve communication and connection with members, map those opportunities to these channels with additional or enhanced member touchpoints.
Remember: The goal is not only to retain these members but also to improve their journey and care management for improved health outcomes.
Strategy in Action: Member and Provider Portals
Having an online hub for members to access important information, get answers to their questions, and take next steps is table stakes. For payers looking to build better member journeys, it’s one of the first touchpoints they should optimize, along with provider portals.
Member portals combine billing, care, benefit programs, and notifications in one intuitive interface. Members can access data across multiple systems in a central, secure location. Payers can deepen relationships with this touchpoint through surfacing relevant information, reminding members to log in for important updates, and streamlining alerts.


Provider portals centralize and deliver prescriptive and consultative analytics, notifications and alerting, and exchange of data. Provider groups, individual providers, and internal users at the health plan access an intuitive, personalized interface to see exactly what action needs to be taken to improve member care.
AI AND AUTOMATION: Many payers uncover recertification periods as a common risk because members are unaware of the timeline and steps to take. When creating a member retention strategy, they may decide to add targeted and timely outreach across multiple channels to ensure members are aware of their responsibility to re-enroll.
With the help of AI and automation, payers can implement technology capable of automatically engaging with more than 700,000 members through omnichannel touchpoints during looming recertification periods. This increases the likelihood that members know of upcoming timelines and take steps to stay covered and cared for.
Predictive analytics takes this technology even further. With the input of well-defined member personas, MCOs can use AI predictive models to automatically search for churn risk parameters, flag at-risk members, and trigger outreach workflows.
PROACTIVE CUSTOMER SUPPORT: Disengagement patterns can signal that a member relationship is weak and that churn is possible, if not likely. Instead of ignoring these warning signs or simply reacting when members reach out for help, a member-centric approach notes disengagement and takes action.
An AArete client implemented proactive retention efforts by defining disengagement parameters. Such patterns automatically triggered customer service intervention for primary care physicians and disease-specific case management assignments. This outreach led to a 33% decrease in new member churn.
UNIFIED ENGAGEMENT PLATFORM: At the core of the member journey should be a single digital source of truth. A Member 360 engagement platform creates a centralized view of each member for customer service, care management, members, and providers.
These platforms bring together data from across channels for all involved stakeholders to access. But perhaps most importantly, they give members the tools to manage their healthcare journey and find the right support at the right time.
The CRM in Action
At the center of your engagement efforts is your CRM. A tool like Salesforce brings together all of the elements of your member retention strategy, offering a central view of members, targeted omnichannel engagement, and ongoing evaluation of engagement and satisfaction. It also allows you to embrace more efficient ways of getting in touch with members based on their unique needs, so you scale your vision for a better member journey across your base.
Choose the Right Priorities
The goalpost for MCOs has moved. Leading MCOs recognize that the real value lies in creating member journeys that are personal, proactive, and outcome-driven. These priorities can lower costs for patients and MCOs alike and, creating more long-term sustainability.
As retention rates improve, payers free up further resources to serve members, enhance their care management, and acquire new members more efficiently for plan growth. By leveraging a CRM like Salesforce to surface insights and identify risk earlier, you can design experiences that meet members where they are. Data becomes the foundation — not just for understanding churn, but for driving more targeted, effective interventions.
AArete helps you unlock more value from your current tools to implement real strategic change that your members can feel. We conduct metric-driven analysis to compare performance to industry standards, then drill down into underlying process gaps to improve performance and increase efficiency.
If you’re ready to build a member retention strategy that delivers the journey your members are waiting for, let’s work together. Reach out today.